Table 1 – Psychopharmacology principles in transplant recipients
Table 2 – Commonly used immunosuppressants: mechanisms, psychiatric adverse effects, and relevant
drug-drug interactions
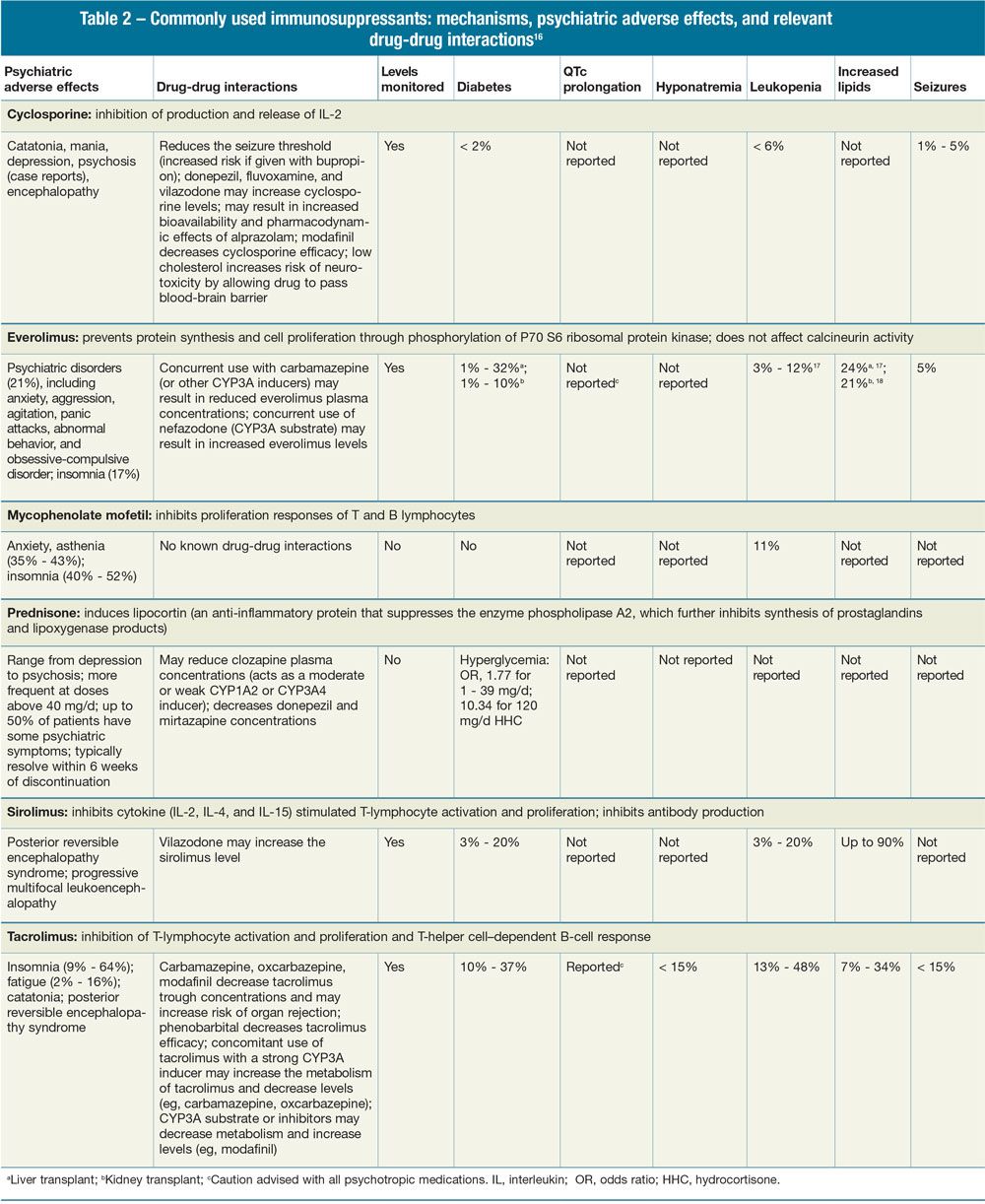
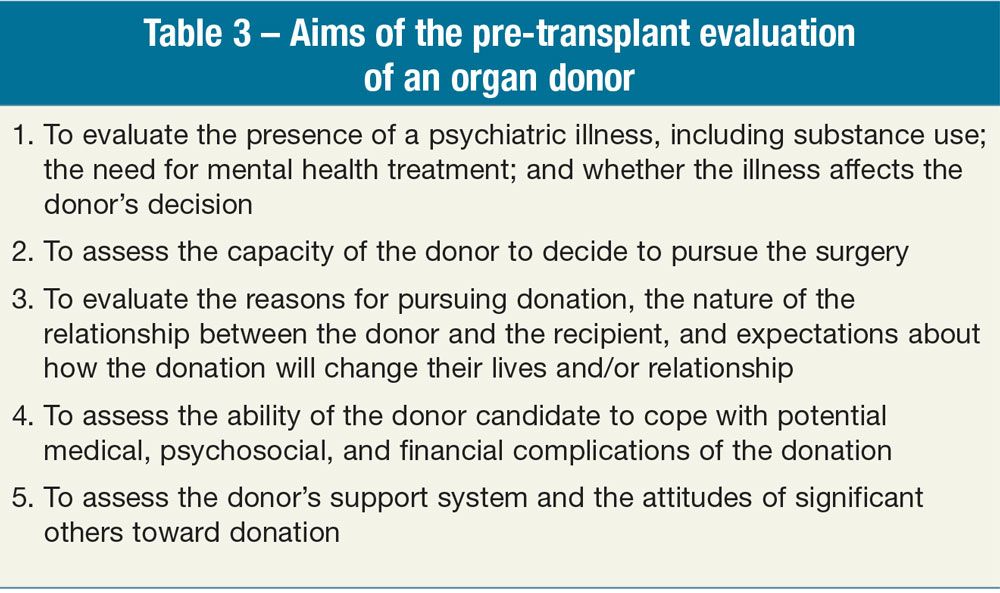
Table 3 – Aims of the pre-transplant evaluation of an organ donor
Academy of Psychosomatic Medicine (APM), Transplant Psychiatry Special Interest Group
Because of the inherent risks and costs associated with transplant in addition to limited organ availability, careful candidate selection is crucial for successful outcomes. Given the prevalence and effects of psychiatric and substance use disorders on quality of life and post-transplant outcomes, the psychiatrist is often called upon to recommend or implement treatment in both pre-transplant and post-transplant stages.
In Part 1 of this article, the various phases of transplant as well as the prevalence and impact of psychiatric illness in the transplant population were discussed.1 Here we review the psychiatric management of transplant patients and the evaluation and care of living organ donors.
Pre-transplant psychiatric management
It is important that preexisting psychiatric conditions are addressed while patients are being evaluated for or are awaiting transplant. In most cases, the early phase of the pre-transplant stage is an optimal time to “fine-tune” mental health treatment. The underlying medical condition is relatively stable, and the patient can still participate in psychotherapy or receive psychopharmacological treatment.
The hope for better quality of life after transplant can motivate patients to pursue mental health treatments that they had previously refused (eg, start addiction treatment, taper off sedatives, participate in psychotherapy). During this phase, mental health care follows the recommendations available for the psychiatric care of the medically ill.2-4 In addition to general psychosomatic care, specific treatments such as transplant-focused stress-reduction interventions can be useful.5,6 As medical illness worsens, additional challenges may interfere with psychiatric care:
• Patients may become too physically ill to participate in mental health treatment.
• Cognitive impairment may prevent meaningful psychotherapy.
• The logistics of intense medical care (hospitalizations for medical decompensations, high number of medical appointments) may interfere with adherence to psychiatric treatment.
Post-transplant psychiatric management
In the acute post-operative setting, psychiatrists are often asked to help diagnose and manage delirium and steroid-induced psychiatric symptoms. Post-transplant delirium is approached by systematic evaluation of risk factors; addressing acute medical conditions that contribute to delirium (such as infection and metabolic disturbances); simplification of the medication regimen whenever possible (eg, reducing dosages of opioids or benzodiazepines); and behavioral interventions (such as minimizing stimulation, promoting access to daylight normalization of sleep-wake cycle, early mobilization, and frequent reorientation). If medications are used, antipsychotics remain the first line of treatment. Antipsychotics can be safely used to treat delirium or steroid-induced psychosis in the post-transplant phase, while patients are monitored carefully for elevated QTc, seizures, hyponatremia, and neutropenia.
Psychotherapy can be implemented as stand-alone treatment or in addition to pharmacology.
In the long term, several studies have documented that depression or psychosis in the post-transplant phase is associated with worse medical outcomes.7,8 For substance use disorder, findings suggest that post-transplant treatment is as important as pre-transplant relapse prevention in helping patients maintain abstinence.9 General considerations regarding pharmacological treatment of organ transplant recipients are outlined in Table 1. The life-long immunosuppressant regimen may lead to psychiatric symptoms, pharmacokinetic interactions with psychiatric medications, or synergistic effects that can alter long-term outcomes (Table 2).
Psychotherapy can be implemented as stand-alone treatment or in addition to pharmacology, provided there is no significant cognitive impairment. Relevant themes for psychotherapy in the post-transplant setting are loss (of time spent ill waiting for an organ, of social status, financial situation); change in social role (from critically ill to quasi-healthy); acceptance of the post-transplant limitations because of medical comorbidities not improved with the transplant (eg, diabetic retinopathy after a kidney transplant); guilt; body image concerns; living with an increased risk of health problems (malignancies, infections); medication adherence; and expressing gratitude toward the donor or his or her family. Many transplantation centers offer counseling focused on improving medication adherence and communicating with the donor or the donor’s family.
Evaluation and management of living organ donors
In addition to caring for patients who undergo transplant, psychiatrists are also asked to evaluate potential living organ donors. This primarily involves those who seek to donate a kidney or a portion of their liver. Donors may be closely related to the potential recipient, such as family or friends (“related donor”), but they can also be peripherally related, such as a co-worker (“unrelated directed donation”), or even someone who is unknown to the recipient and donates anonymously (“non-directed donation”).
Organ donors are carefully screened and at times require adjustments of their psychiatric care before being accepted as donors.
No matter what the nature of the relationship to the recipient, donor evaluations are similar to a pre-transplant candidate evaluation. However, there is greater emphasis on informed consent and determining whether there is coercion, undue psychological pressure, or otherwise unhealthy motivations driving the desire to donate (eg, enhancing self-worth, creating a relationship with the recipient, financial remuneration; Table 3).
Organ donors are carefully screened and at times require adjustments of their psychiatric care before being accepted as donors. An innovative, transplant-specific use of motivation enhancement therapy in living organ donors who express ambivalence about donating may reduce post-surgical physical and psychiatric symptoms.10
Depression is the most common problem in organ donors. The cumulative rate of diagnosed depression in kidney donors was 4.2% at 1 year and 11.5% at 5 years, which is lower than in the general population.11 There is limited information on organ donors with preexisting psychiatric disorders; a small study of 22 kidney donors suggests that organ donation is not followed by psychiatric decompensation.12
After donation, as organ function is recovering, psychotropic medications must be adjusted accordingly. Beyond the recovery period, it is wise to avoid psychotropic medications with direct toxicity (eg, lithium for kidney donors), although there is no clear evidence of a higher risk of toxicity in organ donors compared with the general population.
Conclusions and future directions
Transplant is the optimal treatment for a variety of advanced organ diseases. However, due in large part to the scarcity of available organs, transplant programs must carefully select patients who are most likely to benefit from this procedure.
Organs from living donors help address the gap between the need for and the supply of organs. Because these donors undergo surgery for no personal medical benefit, they must be carefully selected and monitored to minimize their risks.
Psychiatrists play a vital role as team members involved in the selection and care of transplant candidates, recipients, and living donors. Historically, their role has focused on the pre-transplant and perioperative phases of care. However, as the populations of long-term transplant survivors and living donors grow, psychiatrists are likely to be called on more often to provide recommendations, referrals, and care for both recipients and donors.
As the field of transplantation continues to expand, psychiatrists have greater responsibilities for the psychosocial evaluation of transplant and donor candidates, and for ensuring that transplant candidates understand the risks and benefits of deceased donor options and the possibility of living donation.
Post-transplant care of recipients also continues to evolve, with ongoing developments in immunosuppressant options. The neuropsychiatric adverse effects of these medications require careful study, especially during long-term use. Psychiatrists and other mental health professionals play vital roles in documenting the nature of these effects, and in determining whether and when patients need to switch to other therapies.
As the populations of long-term transplant survivors and living donors grow, psychiatrists are likely to be called on more often to provide care.
Novel strategies for behavior interventions also require additional research because transplant recipients often live far from their transplant centers. Effective interventions may need to be offered via telephone or the Internet, rather than through traditional face-to-face encounters.
Finally, new areas of transplantation are evolving, most notably transplant of vascularized composite allografts, including face, limb, and reproductive organ transplants.13 The mental health of individuals who are considered for these types of transplants can be one of the key indicators of need or justification for transplant. For example, the stigma associated with severe, permanent facial injury and disfigurement can be extreme and can lead to profound psychological distress.
Overall, the field of transplantation, as a whole, provides an abundance of opportunities for the psychiatrist as both clinician and researcher to contribute to the knowledge base and to the ongoing care and well-being of individuals undergoing extraordinary treatments.
Acknowledgment-The authors acknowledge Christina Wichman, DO, FAPM, of the Academy of Psychosomatic Medicine (APM) for helping bring this article to fruition. The APM is the professional home for psychiatrists providing collaborative care bridging physical and mental health. Over 1200 members offer psychiatric treatment in general medical hospitals, primary care, and outpatient medical settings for patients with comorbid medical conditions.
Disclosures:
Dr. Zimbrean is Assistant Professor of Psychiatry and Surgery, Director of Transplant Psychiatry Services, and Associate Director of Psychosomatic Medicine Fellowship at Yale New Haven Hospital, New Haven, CT. Dr. Crone is Vice Chair, Department of Psychiatry, Inova Fairfax Hospital, Associate Professor of Psychiatry, George Washington University Medical Center, Washington, DC, and Immediate Past President, Academy of Psychosomatic Medicine. Dr. Sher is Assistant Professor of Psychiatry and Behavioral Sciences at Stanford University and Associate Director of Psychosomatic Medicine Fellowship at Stanford University Medical Center, Stanford, CA. Dr. Dew is Professor of Psychiatry, Psychology, Epidemiology, Biostatistics, and Clinical and Translational Science and Dr. DiMartini is Professor of Psychiatry and Surgery and Associate Professor of Clinical and Translational Science in the Department of Psychiatry at the University of Pittsburgh, Pittsburgh, PA. The authors report no conflicts of interest concerning the subject matter of this article.
References:
1. Zimbrean P, Crone C, Sher Y, et al. An introduction to transplant psychiatry: part 1. Psychiatric Times. 2016;33(9):40A-40C.
2. Levenson J. The American Psychiatric Publishing Textbook of Psychosomatic Medicine: Psychiatric Care of the Medically Ill. 2nd ed. Arlington, VA: American Psychiatric Publishing, Inc; 2011.
3. Fogel BS. Psychiatric Care of the Medical Patient. 3rd ed. New York: Oxford University Press; 2015.
4. Ferrando SJ, Owen JA. Clinical Manual of Psychopharmacology in the Medically Ill. Arlington, VA: American Psychiatric Publishing, Inc; 2010.
5. Gross CR, Kreitzer MJ, Thomas W, et al. Mindfulness-based stress reduction for solid organ transplant recipients: a randomized controlled trial. Altern Ther Health Med. 2010;16:30-38.
6. Ramirez P, Febrero B, Martinez-Alarcon L, et al. Benefits of group psychotherapy in cirrhotic patients on the liver transplant waiting list. Transplant Proc. 2015;47:2382-2384.
7. Dew MA, Rosenberger EM, Myaskovsky L, et al. Depression and anxiety as risk factors for morbidity and mortality after organ transplantation: a systematic review and meta-analysis. Transplantation. 2015;100:988-1003.
8. Abbott KC, Agodoa LY, O’Malley PG. Hospitalized psychoses after renal transplantation in the United States: incidence, risk factors, and prognosis. J Am Soc Nephrol. 2003;14:1628-1635.
9. Rodrigue JR, Hanto DW, Curry MP. Substance abuse treatment and its association with relapse to alcohol use after liver transplantation. Liver Transpl. 2013;19:1387-1395.
10. Dew MA, DiMartini AF, DeVito Dabbs AJ, et al. Preventive intervention for living donor psychosocial outcomes: feasibility and efficacy in a randomized controlled trial. Am J Transplant. 2013;13:2672-2684.
11. Lentine KL, Schnitzler MA, Xiao H, et al. Depression diagnoses after living kidney donation: linking U.S. Registry data and administrative claims. Transplant. 2012;94:77-83.
12. Rowley AA, Hong BA, Martin S, et al. Psychiatric disorders: are they an absolute contraindication to living donation? Prog Transplant. 2009;19:128-131.
13. Jowsey-Gregoire SG, Morelon E, Petruzzo P, Seulin C. The Chauvet 2014 meeting report: psychiatric and psychosocial evaluation and outcomes of upper extremity grafted patients. Transplant. 2016;100:1453-1459.
14. Naderi N, Bakhshandeh H, Ardeshiri M, et al. Hyper-prolactinemia in men with idiopathic dilated cardiomyopathy: does it have any prognostic implications? Res Cardiovasc Med. 2014;3:e19321.
15. Foley KF, Kast RE. Review of evidence that posttransplantation psychiatric treatment commonly affects prolactin levels and thereby influences graft fate. Gen Hosp Psychiatry. 2006;28:230-233.
16. Drug Index. https://www.drugs.com/drug_information.html. Accessed August 29, 2016.
17. Hurst FP, Altieri M, Patel PP, et al. Effect of smoking on kidney transplant outcomes: analysis of the United States Renal Data System. Transplant. 2011;92:1101-1107.
18. Baines LS, Joseph JT, Jindal RM. Emotional issues after kidney transplantation: a prospective psychotherapeutic study. Clin Transplant. 2002;16:455-460.

