A 67 -year -old man who accepted liver transplant in October 2021 revealed the history of fever (peak at 38.3 ° C) to the infectious disease bureau on June 24, 2023. He also reported sore throat, chest tension, mild cough, and SP production production. According to the patient's explanation, he visited another hospital five days ago. At that time, his Covid-19 antigen test was positive, but the nucleic acid test of COVID-19 was negative. As a result, he prescribed 1.125 g Simnotrelvir/300 mg Ritonavir PO Q12H and advised to get an outpatient follow -up. Noticeable, his symptoms did not settle on the five-day Simnotrelvir-Ritonavir course. In addition, as part of the liver transplant plan, he administered 8 mg methylprednizolon, 2 mg of tacrolimus, and 720 mg sodium Maicphenolate every day.
The patient was hospitalized for a total of 44 days. In the meantime, the overall clinical course is shown in Fig. 1, and the treatment course shows the treatment course. BMI of 19.03 kg/m2, temperature 37.8 ° C, 22 breath per breath, blood pressure 120/70 mm/hg, heart rate 108 beats, 108 beats per minute, and 98 % of transcolidated oxygen oxygen (SPO2) 98 % 3 l/min). The computer fault shooting (CT) on the chest showed scattered shadows and support pneumonia. The value of the base line laboratory has revealed the rise of C reactive proteins (73.2 mg/l ↑), interloy chin-6 (66.83 Pg/ml ↑), and ferritin (> 1500 µg/ml ↑). 。 Leukocytes (4.92 × 10)9/L) was within the normal range, but the speed of the neutrophil was controlled upward (92.1 % ↑). The porimerase chain reaction of the cotton swab was negative to the COVID-19 and the respiratory pathogen panel (containing nine respiratory infectious viruses, Mycoplasma pneumoniaand Chlamydia) Considering the patient's immunosuppressive status and the rapid progress of the pulmonary imaging, a bronchoscopy is conducted, 70 mg Caspofanging IV QD (50 mg after the second day) and 320 mg trimet prim (TMP)/ 1600 mg Sulfamethoxazole (SMX) PO Q8H was Q8H. Started to cover possible fungus P. Jirovecii The first day. In addition, the immunosuppressive regimen has been discontinued.
Patient clinical and laboratory findings and results. This number is important for chest CT, MNGS results, culture results (1 –3) -a-D-glucan test, galactman nannan (GM) test, oxygen saturation level, oxygen saturation level, and hospitalization of patients. The test result was shown. Body temperature
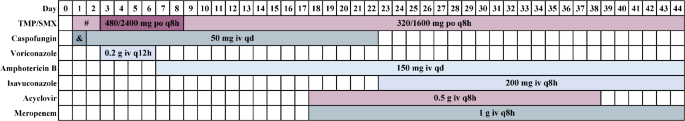
Outline of patient treatment course. TMP /SMX: Trimetoprim /Sulfamethoxazole. The symbol ” #” represents “320/1600 mg PO Q8h”. The symbol “&” represents “70 mg IV QD”
On the third day, the patient's respiratory condition worsened, causing dyspnea. The temperature was 38.8 ° C, and the oxygen saturation was 94 % while the patient breathed via the nose cannula (5 L/min). Standard low -flow nasal oxygenization has been changed to high -flow nasal cannula oxygen therapy (HFNC). BALF Metagenom Next Generation Sequence (MNGS) Analysis has returned to positive B. BRONCHISEPTICA (63266 reading), P. Jirovecii (64746 reading) and A. FUMIGATUS (453 Reads), Human Alphaherpesvirus 1 (HSV1) (128 Reads). BALF's Galactomannan (GM) test is 1.46 S/CO, and serum GM test is 0.22 S/Co. [1–3]-β-D-glucan test was 60.3 PG/mL. 0.2 G Boliconazole IV Q12H has been added to the antibiotic therapy and the dose of TMP/SMX has been increased to 480 mg/2400 mg PO Q8H. Balf culture has been revealed (A) Fumigatus complex Growth and exhibition (B) Bronchiseptica (Two days after being reported by MNGS). Drug -sensitive data B. BRONCHISEPTICA Supplements displayed in the table E1.
After 5 days of treatment by Boliconazole and TMP/SMX, patients developed hearing and visual hallucinations, and aphasia, with serious emotional upset, and cooperating with medical treatment such as oxygen inhalation and blood sampling. I refused. The above symptoms seemed to have been caused by Boliconazole and have recently been added to the treatment regimen. After canceling Boliconazole and changing to 150 mg An Hotelicin B liposomes IV QD (7th day), his hearing and visual hallucinations disappeared, but he was upset. Therefore, the dose of TMP/SMX was returned to 320/1600 mg PO Q8H (9th day).
At the hospital on the 12th day, the patient's mental illness eventually disappeared while body temperature was rising to 39.1 °. High -flow nasal cannula (HFNC) therapy is continuously administered. A bronchoscopy was conducted, and it was reported that the positive BALFMNGS test was positive. B. BRONCHISEPTICA (859 reading), P. Jirovecii (10298 read) and HSV1 on the 13th day (122381 reading). Infection A. FUMIGATUS Effectively controlled. However, the number of HSV1 sequences has increased significantly and suggests the existence of viral pneumonia. The 0.5 g of the Ascloville IV Q8H was started as a treatment for HSV1 infection, and 1 g of Melo Penem IV Q8H was launched as a prophylactic treatment plan for bacterial infection.
Despite the escalating antibiotic therapy, the patient suddenly developed acute respiratory syndrome (ARDS) by the 21st day of the hospital. Immediate resuscitation measures were taken, and the patient was transferred to ICU after the intravenous intubation. The chest CT indicated that both lungs have greatly reduced their spots and integrated pulmonary transparency. There is a double -sided pleural water with partially unrivable uninhabited leaves of both lungs due to compression. The patient's condition did not improve and other microorganisms were suspected. Supplementary blood MNGS has been implemented, and infection has been revealed. C. Elegance。 Serum results [1–3]-β-D-glucan test was 322.5 PG/mL. His regimen has been changed to 200 mg Icab Conazole IV Q8H, 320/1600 MGTMP/SMX PO Q8H, 150 mg AMPHOTERICIN B liposomes IV QD, 1 g melope Nenem IV Q8H, and 0.5 g's Asclonic IV Q8H. The use of Caspofungin has stopped.
After that, a bronchoscopy was conducted (on the 32nd day), and white fungi patches scattered on the lower right leaves under the microscope are scattered. Indicated the growth of the cleaning solution culture C. Elegance (10 days after it is reported by MNGS). Twenty days after treatment, follow -up CT scans showed significant improvements in both pulmonary pulmonary edema, almost completely solved. A thick wall cavity was observed on the right lung, probably related to fungal infections. At the same time, the oxygen of the patient was significantly improved and stable. CT scans in other body parts did not show evidence of the spread of infectious diseases. The patient was still having intermittent fever, but his condition was stable, and he was discharged from a lower hospital for further care (on the 44th day).

