The liver performs hundreds of functions essential to human health. Produces bile, which aids in digestion. Processes nutrients, drugs, and hormones. Makes proteins for blood clotting. Removes toxins from the blood. and regulate the immune response. The liver also has regenerative properties, but when the damage caused by disease exceeds the organ's own healing limits, the consequences can be devastating.
Before the 1960s, liver failure was always fatal. However, in May 1963, Dr. Thomas E. Starzl completed a medical history at the hospital. veterans hospital When he performed the first liver transplant in Denver, Colorado, on a patient who survived surgery. The patient, William G. Grigsby, a 48-year-old janitor, was admitted to a local hospital with symptoms suggestive of peptic ulcer disease. Exploratory surgery revealed that the cancer had covered about a third of his liver, although it had not spread. As his health rapidly deteriorated, he was taken to a Veterans Affairs hospital for a transplant. His donor was a 55-year-old military veteran who had just died of a brain tumor.
The results were short-lived, and Grigsby died a few weeks later from complications from the surgery. But his new liver remained functional until the end. This case provided a glimmer of hope, demonstrating that it is indeed possible to replace a diseased liver with a healthy liver from a donor. We also got a glimpse of the future. Eventually, after another two decades of research and trials, much of it led by Starzl himself, liver transplantation fulfilled its promise and became a reliable life-sustaining treatment for children and adults suffering from end-stage liver disease.
Starzl's experimental work on liver transplants in dogs early in his career convinced him that the same procedure could be performed on humans. A Navy veteran, he earned his medical degree and doctorate from Northwestern University School of Medicine in Chicago in the early 1950s.
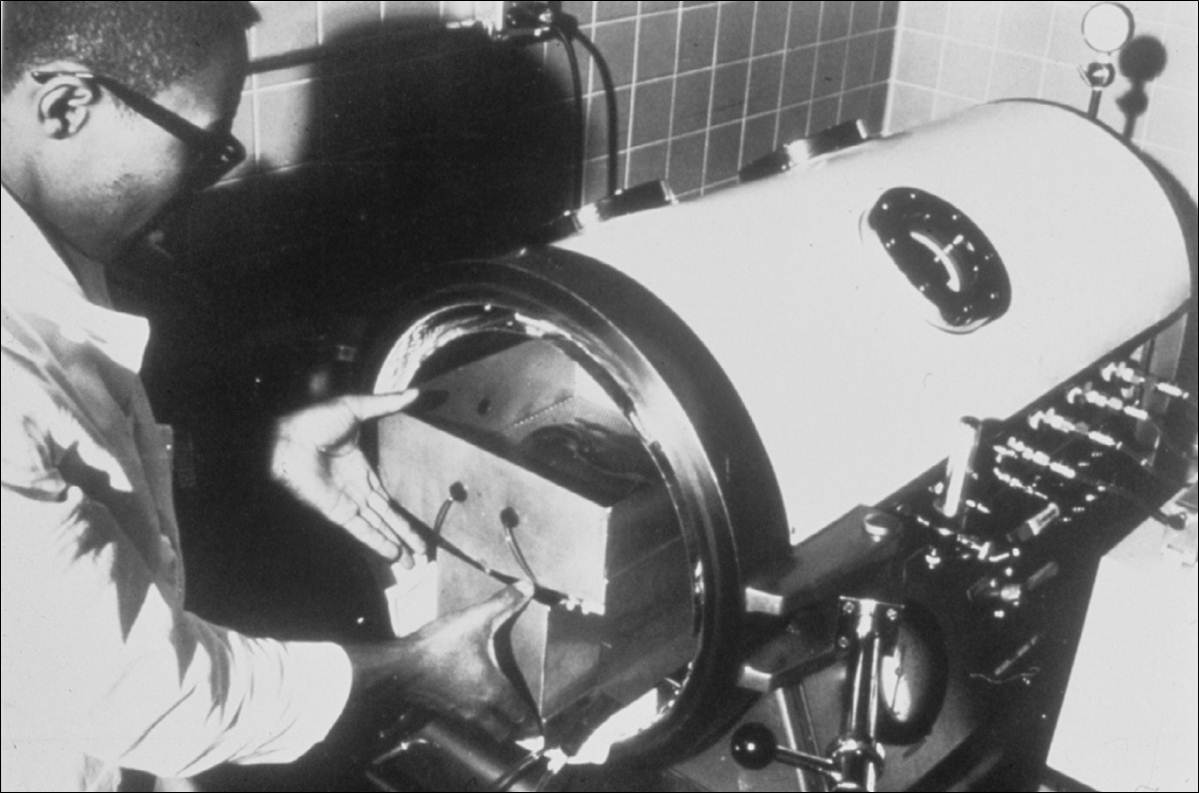
He returned to Chicago in 1958 and worked as a resident surgeon at the Chicago Veterans Affairs Medical Center. There he began a research program using dogs, which he expanded a year later when he joined Northwestern University's Department of Surgery. While at Northwestern University, he performed 79 liver transplants on canine subjects. These experiments generated important knowledge about surgical techniques for preserving donor livers and redirecting blood flow, which turned out to be the basis for the emerging field of solid organ transplantation.

In late 1961, Starzl accepted a new position as chief of surgery at the Denver Virginia Hospital. His veteran salary paid for his concurrent position at the University of Colorado School of Medicine. As Starzl recalled in his 1992 autobiography, he was recruited to the school's Department of Surgery for the overriding purpose of “bringing liver transplantation to clinical use.”
But he began with a kidney transplant, an operation that surgical teams elsewhere had been completing with intermittent success starting in 1954. Starzl quickly surpassed those early efforts thanks to a new drug protocol that reverses the effects of organ rejection. This immunosuppressive therapy was derived from his ongoing experiments with dogs at the Veterans Affairs Research Institute in Denver. From November 1962 to March 1964, he performed 64 living donor kidney transplants. A subsequent analysis of kidney transplant registries conducted in 1989 found that 15 of the original patients in this group were still alive.
Liver transplants pose a much more complex challenge, and Starzl's first surgical attempt in March 1963 failed, with the patient dying on the operating table. Two months later, he tried again with William Grigsby. Starzl and his team performed the historic transplant on May 5, 1963. One week after surgery, Grisby was able to sit up and eat on his own. However, his condition worsened two weeks later, and he died on May 27 of pneumonia caused by a respiratory infection.
Starzl underwent three more liver transplants in 1963, with the same results. The patient survived for up to 23 days but died from a postoperative infection. However, in all four cases, autopsy results showed good liver function and few signs of organ rejection.
Dr. Starzl took a four-year hiatus from the liver transplant program and refocused his research with dogs at the Veterans Affairs Laboratory. This research has led to advances in surgical techniques, postoperative care, and medications to reduce the risk of rejection.
He resumed transplant surgery in 1967 and performed transplants on 165 patients from 1967 to 1979. The overall 1-year survival rate was only about 33 percent, but the outcome was much better, with 18 patients surviving more than 20 years. In 1979 and 1980, Starzl and European researchers achieved a series of breakthroughs in immunosuppressive treatments that dramatically improved the prognosis of transplant patients. The one-year survival rate jumped to 70%. In 1981, Starzl moved the program to the University of Pittsburgh, where he established what quickly became the world's premier liver transplant center.
In a paper published in 1982, Dr. Starzl reflected on the long and winding journey that led to his pioneering research in liver transplantation, writing, “If you look at the history of medicine, yesterday it was unthinkable, today it is barely possible.'' “What is achieved often becomes routine tomorrow.” By the time he retired from clinical practice in 1991, liver transplants had become routine in practice, and transplant centers were opening across the country. More than 100 hospitals in the United States now offer this service, including six in Virginia, and about 75 percent of transplant recipients survive for more than five years.