Patient characteristics
Baseline characteristics of the study population are shown in Table 1. A total of 8,764 patients were included, of whom 7,725 (88%) received his rATG and 1,039 (12%) received her PTCy as her GVHD prophylaxis.
Overall, the majority of patients were transplanted for acute leukemia (58%), myelodysplastic syndromes (MDS) (19.7%), myeloproliferative neoplasms (MPN) (9.7%), or lymphoma (9%). I did. A high proportion of patients had a low/intermediate disease risk index (DRI, 72.1%), and myeloablative conditioning (MAC) was performed more frequently than reduced-intensity conditioning (RIC). (53.3%).
Patients in the rATG group were older, with a median age of 58.6 years (IQR (48.1, 65.4)), whereas patients in the PTCy group were 53 years (IQR 38.6, 62.3) (p< 0.01), and a similar proportion of men (57.3% for rATG and 58.9% for PTCy) p= 0.33), significantly reduced the use of TBI (14.5% vs. 24.7%; p< 0.01) and lower MAC utilization (52% vs. 62.3%, p< 0.01). The PTCy group also had a lower disease recurrence index and a more recent year of transplantation (Table 1). The remaining parameters were balanced between the two groups. Median follow-up was 2.1 years in both arms. More detailed information is shown in Table 1.
Survival, RI, NRM
Univariate results are shown in Figures 1 and 2. The results of the multivariate analysis are summarized in Table 3. P– The values and hazard ratios (HR) shown in the results section below are obtained from multivariate analysis.
a NRM; B overall survival, C incidence of recurrence, D progression-free survival and E GVHD-free recurrence-free survival. The cumulative incidence is displayed.
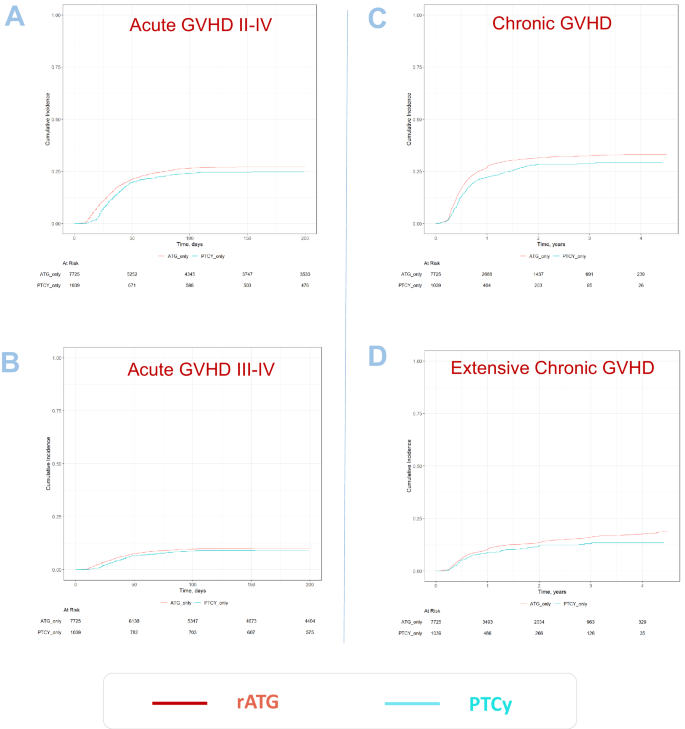
a Acute GVHD grade II-IV. B Acute GVHD grade III-IV; C Chronic GVHD all grades and D Extensive chronic GVHD – Cumulative incidence is shown.
Patients who received PTCy had significantly lower NRM compared to those who received rATG (2-year incidence: 12.4% vs. 16.1%, HR: 0.72) [95% CI 0.55–0.94], p= 0.016). Similarly, OS and PFS showed a statistically significant and clinically meaningful benefit in the PTCy treatment group, with higher OS (2-year incidence: 73.9% vs. 65.1%, HR: 0.82). [95% CI 0.72–0.92], p= 0.001), higher PFS (2-year incidence: 64.9% vs. 57.2%; HR: 0.83) [95% CI 0.74–0.93], p< 0.001). RI was lower in the PTCy group (2-year incidence: 22.8% vs. 26.6%, HR: 0.87) [95% CI 0.75–1.00], p= 0.046).
The causes of death are shown in Table 4. No significant differences were found between the two groups. Recurrence of the underlying malignancy was the most frequent cause of death, accounting for approximately 50% of all deaths in both groups, followed by NRM causes: infections approximately 18%, GVHD approximately 16%, and other allogeneic SCT-related causes overall. approximately 8% of deaths (number of deaths). Secondary malignancies contributed to approximately 1% of total deaths.
Incidence of acute and chronic GVHD, and GRFS
Overall chronic GVHD was lower in the PTCy group (2-year incidence: PTCy 28.4% vs rATG 31.4%, HR: 0.77) [95% CI 0.63–0.95], p= 0.012). Extensive chronic GVHD was also reduced in patients who received PTCy compared to rATG: (2-year incidence: 11.9% vs. 13.5%, HR: 0.75) [95% CI 0.62–0.91], p= 0.004).
The incidence of grade II-IV acute GVHD in patients receiving PTCy was not statistically significant compared to patients receiving ATG: (100-day incidence: 24.1% vs. 26.5% ; HR: 0.85 [95% CI 0.69–1.04], p= 0.11). Similarly, severe acute GVHD grade III to IV (100-day incidence: 8.7% vs. 9.7%; HR: 0.76) [95% CI 0.55–1.05], p= 0.091).
GRFS was significantly higher in the PTCy group compared to the rATG group (2-year incidence: 51% vs. 45%, HR: 0.86) [95% CI 0.75–0.99], p= 0.035).
Neutrophil recovery and incidence of second allogeneic SCT
The EBMT database does not contain data on transplant failure/rejection. We investigated neutrophil recovery after first allogeneic SCT and the incidence of second allogeneic SCT to gain insight into initial transplantation success and subsequent need for additional transplantation procedures. The median incidence of neutrophil recovery at days +30 and +60 in the ATG vs. PTCy group was: d + 30 ATG 96% (IC95% 95.5-96.4) vs. PTCy 91% (89 ~92.7) and d + 60 ATG 97.9% (97.6 to 98.2) vs. PTCy 97.4% (96.2 to 98.3). The median incidence of a second allogeneic SCT at 2 years was 4.3% (3.8 to 4.8) in the ATG group and 3.2% (2.2 to 4.6) in the PTCy group.

